
Charite Team gives Background on Chronic Wounds
Chronic Wounds – Background Interview with Fiorenza Rancan
NABIHEAL is a Horizon Europe project that will develop multifunctional biomaterials to improve wound management. Within the project, partner Charité – Universitätsmedizin Berlin leads the work package in charge of the in vitro, ex vivo, and in vivo tests for the efficacy evaluation. Charité uses ex vivo wound infection models to evaluate the antimicrobial activity of the new biomaterials developed during the project selected through in vitro antimicrobial and wound healing tests.
Figure 1 (titleimage): Fiorenza Rancan (second from right), Annika Vogt (right) and the NABIHEAL team from Charité.
We sat down with Fiorenza Rancan, Senior Research Investigator and Martina Hüging, Head of paediatric plastic surgery, congenital vascular malformations and haemangiomas (IZG), at Charité in Berlin, to learn more about chronic wounds.
Although, we knew chronic wounds present a problem, we were taken aback to hear about the actual incident rate. Yet it is still a problem that is seldom discussed in the media. Why is that?
People with chronic wounds often feel ashamed and prefer to avoid the subject. For the media, it may not be an attractive subject because there is no real breaking news about new therapies or insights into the mechanisms underlying the disease.
Nevertheless, the numbers of affected patients are growing: among patients over the age of 60, between 0.6-3 percent suffer from leg ulcers, while in the group over the age of 80 more than 5 percent are affected[1]. In 2019, an average prevalence of 10% was reported for pressure ulcers in European hospitals[2]. Burns can also become chronic, especially when they get infected, which is the case in approximately 30% of burn patients[3].
One of the main reasons for this increase is that the average age of the world’s population is rising and the rates of conditions such as diabetes, venous insufficiency and immobility increase in the older population.
The economic burden for the patients and the healthcare system is increasing too. Thus, more awareness is needed. For example, the prevention of wounds or wound infection is certainly an important aspect that should receive more attention in the media. It is of particular importance to provide information and raise awareness among those patients who are predisposed to developing chronic wounds, e.g. immunocompromised and diabetic patients.
Can you describe what leads to chronic wounds?
A chronic wound is a wound in which the healing process is either arrested or significantly delayed as a result of a general alteration of the wound environment and of one or more of the several processes contributing to the healing process. In acute wounds, damage is repaired by a variety of cell types that are activated by a well-balanced proliferative environment, which is rich in nutrients, growth factors, and other signalling molecules. These cells build new tissue and a new skin barrier while the immune system is tasked with preventing the eventual invasion of microorganisms.
If the wound environment is altered due to the absence of essential nutrients and vital signals and the inflammation continues due to the persistence of microorganisms and biofilm, then the repair process will be either impaired, leading to scarification, or delayed.
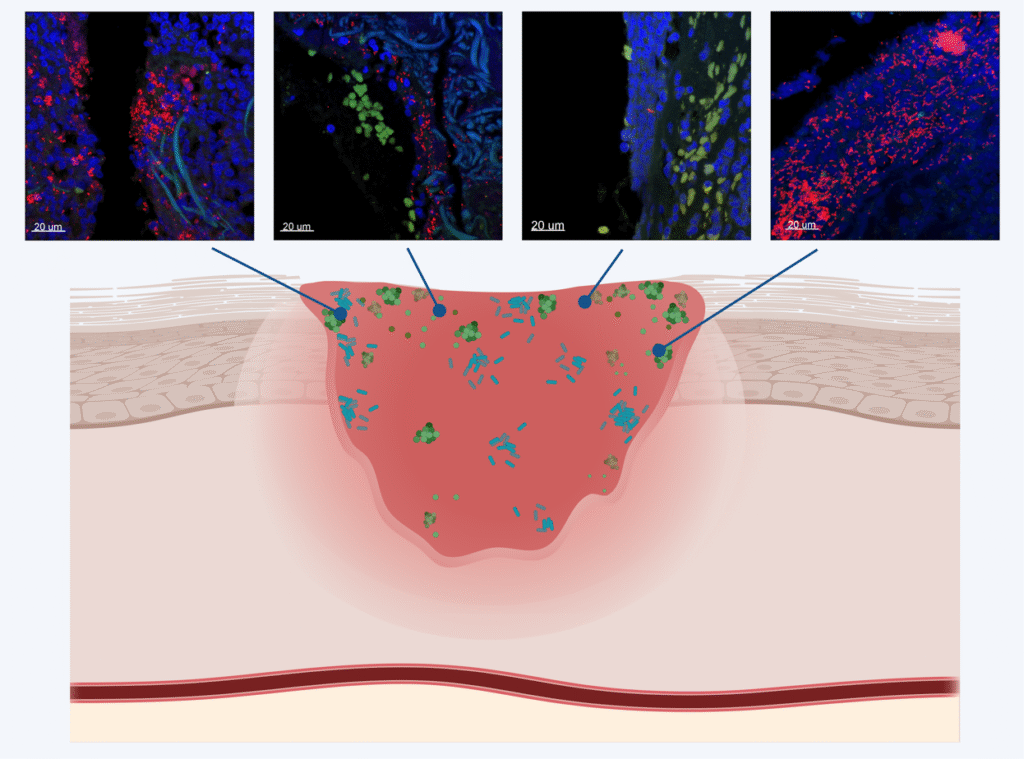
Figure 2: Schematic drawing of a chronic wound with different species of bacteria heterogeneously distributed in various sizes of biofilms and as single cells from the top to the deeper layers of the wound. These figures were created using Biorender.com and are courtesy of the Costerton Biofilm Center, University of Copenhagen.
Are there reasons that make people more prone to chronic wounds?
Patients with pathologies that lead to damage to the blood vessels (arteries and veins), which are responsible for the correct perfusion of blood to and from the skin, are predisposed to developing chronic wounds.
Venous insufficiency is characterised by reduced blood flow in the lower legs, which results in a lack of adequate nutrient supply to the skin. This leads to the development of fragile skin tissue, increasing the risk of developing chronic wounds.
Diabetes is associated with the generation of free radicals, which in turn leads to damage to both peripheral nerves and blood vessels. As a consequence, skin becomes more fragile and it is more susceptible to wounds, particularly at the ankle and foot sole level.
Pressure ulcers are the result of damage to tissue and vessels caused by pressure, which is mainly the consequence of prolonged periods of immobility.
All these conditions are widespread in the population over the age of 60 and their prevalence increases with age.
Immunosuppression is another important aspect. Patients treated with immunosuppressive drugs such as corticosteroids or antirheumatic drugs suffer from delayed wound healing. Oncology patients also have a predisposition to get chronic wounds due to the negative effects of radiation therapy or anticancer drugs that can interfere with the cells of the immune system or even with fibroblasts, which are key cells in the wound healing process.
Can you explain the role of biofilm in chronic wounds?
Microorganisms have the tendency to attach to surfaces, aggregate, and build a slimy matrix that protects them from the environment and the immune system. Such a microorganism community is called biofilm. Biofilms are widespread in nature and can be found for example on rocks, water pipes, washing machines. In the medical setting, they are found on catheters, implants or teeth, etc. and in approximately 80% of chronic wounds. They are very persistent and can negatively impact the wound healing. If they are not removed, they can cause severe infections. The biofilm is typically treated by repeated irrigation of the wound with disinfectants and surgical removal of fibrin, debris, and infected tissue by a technique called debridement. The development of better methods for preventing or removing biofilm in the wound bed is of crucial importance in modern wound management.
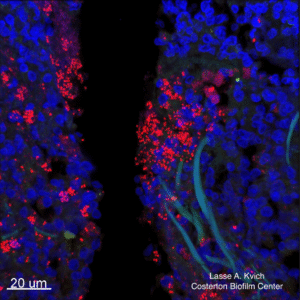
Figure 3: Chronic wound infection, CLSM, 63x, S. aureus. Courtesy of the Costerton Biofilm Center, University of Copenhagen.
There seems to be a lack of knowledge among not-specialized healthcare workers about how to deal with chronic wounds. Is wound healing and wound care an especially difficult subject in medicine?
Patients with chronic wounds have complex underlying clinical patterns. Wounds can have different aetiologies, and different stages of healing and tissue environments must be recognised within the same wound.
However, there is also a lack of knowledge that is not due to the difficulty of the subject. The main problem is that chronic wounds do not fit to any specific field of medicine and, thus, for years there were no specific courses for physicians and nurses to train and get certified on this subject. In the last years this has been improved, especially thanks to wound care societies, but there is still more room for improvement.
Tell us about the most common wound healing materials available currently – and what made you and your team want to develop something better?
A wide variety of materials are used in wound healing.
Most of the currently used dressings aim at maintaining a moist environment and at managing the wound exudate. Films, foams, hydrocolloid dressings, hydrogels, alginate dressings are used at this purpose. Other dressings improve the healing process thanks to antioxidative or matrix-building molecules. One dressing may be preferred over another depending on the type of wound or the stage of wound healing.
Controlling wound bacteria is also critical. If the bacterial count is low and there are no symptoms, a wound is said to be colonised. Conversely, if the bacteria count is high and there are symptoms such as redness, swelling, pain or fever, the wound is considered infected. Such a wound, or any wound at risk of infection, should be treated with an anti-microbial agent. However, in many chronic wounds, systemic antibiotic treatment is not effective due to poor blood circulation and tissue perfusion. Local antimicrobial treatments are therefore necessary. Silver dressings or antimicrobial wound gels are commonly used. However, such treatments are not free of side effects and may slow down the wound healing process.
Within NABIHEAL, our team aims to develop wound treatments that can improve the different aspects of the wound healing process by simultaneously preventing wound colonization and/or infection. Antimicrobial agents are often toxic to both bacteria and human cells. A treatment with preferential antimicrobial effect with low cell toxicity holds the promise to improve the outcome of chronic wounds.
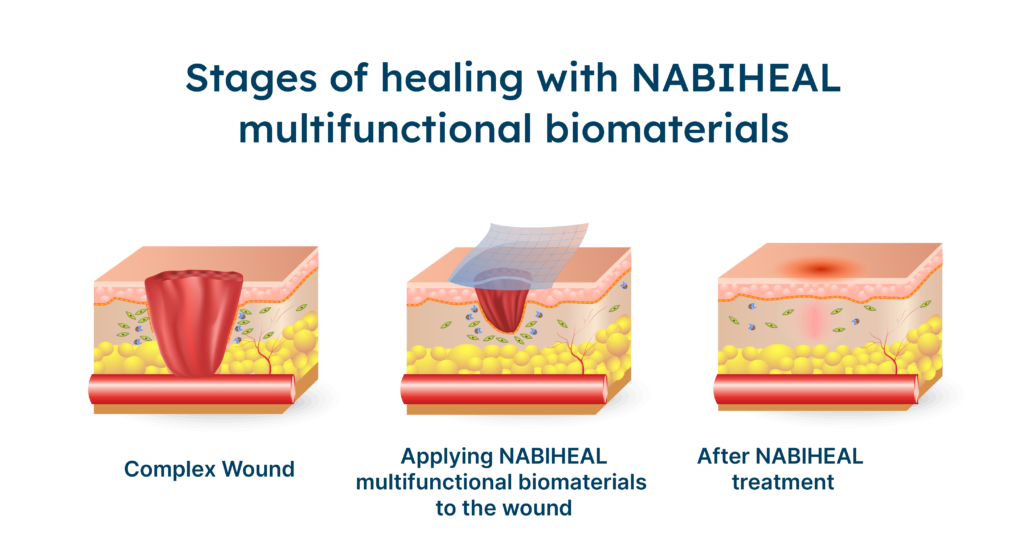
Figure 4: Schematic image of wound healing process with NABIHEAL multifunctional biomaterals.
If the wound healing materials developed in NABIHEAL are successful, what kind of impact will this have – for clinicians as well as patients?
NABIHEAL is developing new materials for the management of different types of chronic and complex wounds at all stages of the wound healing process. All of these different dressings will have additional antimicrobial activity to control wound colonisation and prevent wound infection. If successful, these dressings will give clinicians further options in the management of chronic wounds, particularly in terms of infection prevention.
[1] Rayner R., Carville K., Keaton J., Prentice J., and Santamaria X. N., Leg ulcers: atypical presentations and associated co-morbidities, Wound Practice and Research. (2009) 17, no. 4, 168–185.
[2] Moore, Zena, et al. “The prevalence of pressure ulcers in Europe, what does the European data tell us: a systematic review.” Journal of wound care 28.11 (2019): 710-719.
[3] Mayhall CG. The epidemiology of burn wound infections: then and now. Clin Infect Dis. 2003 ;37(4):543-50. doi: 10.1086/376993

